Despite a decade of mass-drug campaigns and school deworming, new mapping and surveillance, show soil-transmitted helminth (STH) infections remain widespread across Rwanda, with an estimated national prevalence well above thresholds for concern and hotspots in several districts. Public-health experts warn that sustained investment in water, sanitation and targeted treatment is needed to turn the tide.
A national remapping of intestinal worms published in 2025 found that about 38.7% of surveyed people carried at least one species of soil-transmitted helminth (Ascaris, Trichuris or hookworm), with adults often showing higher prevalence than children in some areas, a stark reminder that STH remains a public-health challenge in Rwanda. Species-level results from the study show Ascaris lumbricoides at ~27.0%, Trichuris trichiura ~11.6%, and hookworm ~10.7%. PLOS
Rwanda’s Ministry of Health and the Rwanda Biomedical Centre (RBC), include STH among priority neglected tropical diseases and have run integrated control efforts, notably school-based preventive chemotherapy and community mass drug administration (MDA) in high-risk zones. Despite these programs, recent field surveys and routine health data indicate persistent transmission in many districts, driven by gaps in sanitation, unsafe water, and local variations in program coverage. rbc.gov.rw+1.
What the numbers mean.
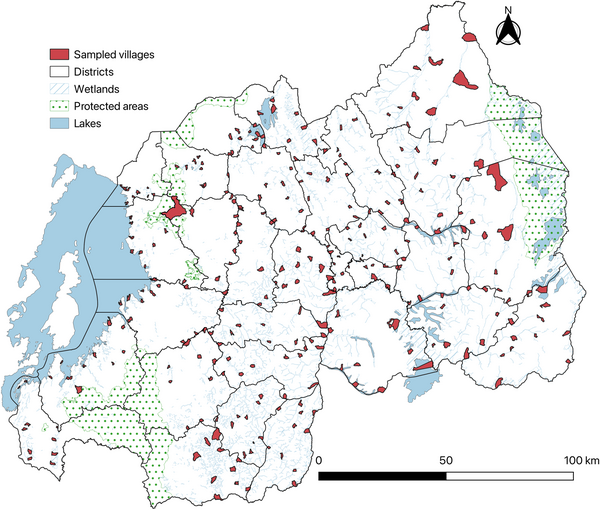
Global guidance classifies STH as a public-health problem where moderate-to-high intensity infections exceed a given threshold; elimination as a public-health problem generally requires sustained reductions in moderate-to-heavy infection levels and strong WASH (water, sanitation, hygiene) improvements. The remapping effort used community and school surveys to produce village-level risk maps, showing that while some areas have seen marked declines, others still post high prevalence and require continued targeted interventions. PLOS+1.
Voices from the field
Health-facility reports and small community studies corroborate the national picture: districts near wetlands and irrigation zones, where people have frequent contact with contaminated soils and water, report higher rates of infection. Local clinicians note that schoolchildren still present with chronic abdominal pain, malnutrition and poor school performance, classic consequences of heavy worm burdens, even after rounds of albendazole or mebendazole. Recent clinical evaluations of single-dose albendazole in Rwanda underline that drug efficacy and reinfection dynamics must both be considered when interpreting MDA results. Rwanda FDA+1
Why STH persists
Public-health researchers emphasise three main reasons: (1) reinfection after treatment because environmental contamination persists; (2) unequal program reach (some communities miss MDA or have low school enrolment); and (3) limitations in sanitation and safe water access that allow transmission to continue. The 2019–2024 Rwanda NTD Strategic Plan calls for combining preventive chemotherapy with WASH improvements, community engagement, and strengthened surveillance, but recent literature recommends sharpening targeting using the new high-resolution maps to concentrate resources where the burden is greatest. rbc.gov.rw+1.
Policy and financing challenges
Experts warn that as international donor attention shifts, domestic financing and program integration will be crucial for sustainability. A 2025 analysis of Rwanda’s approach to financing NTD services highlights the need to embed STH control into routine primary health care and school health platforms and to monitor impact with robust sentinel surveillance.
What would success look like?
Control programs aim to reduce moderate-to-heavy intensity infections to below public-health thresholds and ultimately interrupt transmission in focal areas. That requires continued rounds of preventive chemotherapy targeted by up-to-date mapping; investments in household sanitation and safe water; health education to reduce exposure; and routine monitoring that combines facility data with periodic community surveys. WHO guidance underlines that single interventions are not enough, a package approach is required.